Diagnosis

A complete neurological exam and medical history are needed to diagnose MS.
There are no specific tests for MS. Instead, a diagnosis of multiple sclerosis often relies on ruling out other conditions that might produce similar signs and symptoms, known as a differential diagnosis.
Your doctor is likely to start with a thorough medical history and examination. Your doctor may then recommend:
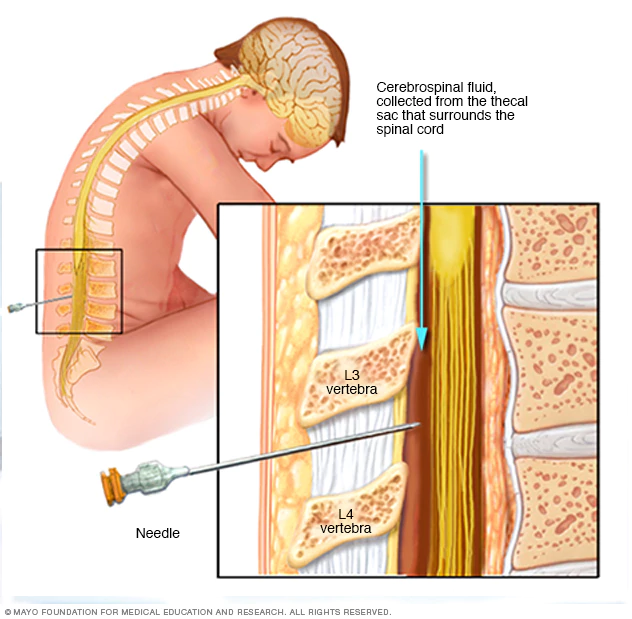
Lumbar puncture (spinal tap)
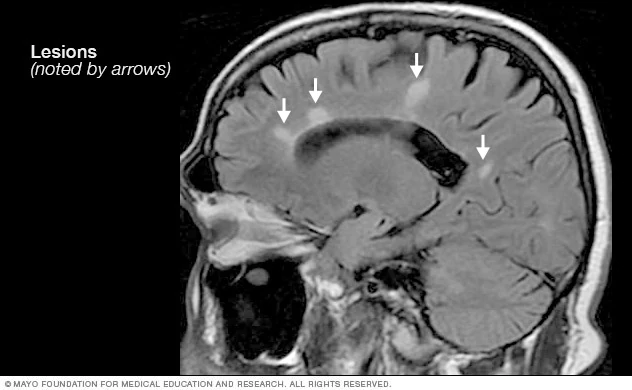
Multiple sclerosis MRI scan
- Blood tests, to help rule out other diseases with symptoms similar to MS. Tests to check for specific biomarkers associated with MS are currently under development and may also aid in diagnosing the disease.
- Lumbar puncture (spinal tap), in which a small sample of fluid is removed from your spinal canal for laboratory analysis. This sample can show abnormalities in antibodies that are associated with MS. Spinal tap can also help rule out infections and other conditions with symptoms similar to MS.
- MRI, which can reveal areas of MS (lesions) on your brain and spinal cord. You may receive an intravenous injection of a contrast material to highlight lesions that indicate your disease is in an active phase.
- Evoked potential tests, which record the electrical signals produced by your nervous system in response to stimuli. An evoked potential test may use visual stimuli or electrical stimuli, in which you watch a moving visual pattern, or short electrical impulses are applied to nerves in your legs or arms. Electrodes measure how quickly the information travels down your nerve pathways.
In most people with relapsing-remitting MS, the diagnosis is fairly straightforward and based on a pattern of symptoms consistent with the disease and confirmed by brain imaging scans, such as MRI.
Diagnosing MS can be more difficult in persons with unusual symptoms or progressive disease. In these cases, further testing with spinal fluid analysis, evoked potentials and additional imaging may be needed.
 Brain MRI is often used to help diagnose multiple sclerosis
Brain MRI is often used to help diagnose multiple sclerosisDr. B. Mark Keegan explains the diagnosis and treatment of multiple sclerosis
Treatment
There is no cure for multiple sclerosis. Treatment typically focuses on speeding recovery from attacks, slowing the progression of the disease and managing MS symptoms. Some people have such mild symptoms that no treatment is necessary.
 Multiple sclerosis research laboratory
Multiple sclerosis research laboratoryTreatments for MS attacks
- Corticosteroids, such as oral prednisone and intravenous methylprednisolone, are prescribed to reduce nerve inflammation. Side effects may include insomnia, increased blood pressure, mood swings and fluid retention.
- Plasma exchange (plasmapheresis). The liquid portion of part of your blood (plasma) is removed and separated from your blood cells. The blood cells are then mixed with a protein solution (albumin) and put back into your body. Plasma exchange may be used if your symptoms are new, severe and haven't responded to steroids.
Treatments to modify progression
For primary-progressive MS, ocrelizumab (Ocrevus) is the only FDA-approved disease-modifying therapy. It slows worsening of disability in people with this type of MS.
For relapsing-remitting MS, several disease-modifying therapies are available.
Much of the immune response associated with MS occurs in the early stages of the disease. Aggressive treatment with these medications as early as possible can lower the relapse rate and slow the formation of new lesions.
Many of the disease-modifying therapies used to treat MS carry significant health risks. Selecting the right therapy for you will depend on careful consideration of many factors, including duration and severity of disease, effectiveness of previous MS treatments, other health issues, cost, and child-bearing status.
Treatment options for relapsing-remitting MS include:
Beta interferons. These medications are among the most commonly prescribed medications to treat MS. They are injected under the skin or into muscle and can reduce the frequency and severity of relapses.
Side effects of beta interferons may include flu-like symptoms and injection-site reactions.
You'll need blood tests to monitor your liver enzymes because liver damage is a possible side effect of interferon use. People taking interferons may develop neutralizing antibodies that can reduce drug effectiveness.
Ocrelizumab (Ocrevus). This humanized immunoglobulin antibody medication is the only DMT approved by the FDA to treat both the relapse-remitting and primary progressive forms of MS. Clinical trials showed it reduced relapse rate in relapsing disease and slowed worsening of disability in both forms of the disease.
Ocrevus is given via an intravenous infusion by a medical professional. Side effects may infusion-related reactions including irritation at the injection site, low blood pressure, fever, and nausea among others. Ocrevus may also increase the risk of some types of cancer, particularly breast cancer.
- Glatiramer acetate (Copaxone). This medication may help block your immune system's attack on myelin and must be injected beneath the skin. Side effects may include skin irritation at the injection site.
- Dimethyl fumarate (Tecfidera). This twice-daily oral medication can reduce relapses. Side effects may include flushing, diarrhea, nausea and lowered white blood cell count.
Fingolimod (Gilenya). This once-daily oral medication reduces relapse rate.
You'll need to have your heart rate monitored for six hours after the first dose because your heartbeat may be slowed. Other side effects include headache, high blood pressure and blurred vision.
- Teriflunomide (Aubagio). This once-daily medication can reduce relapse rate. Teriflunomide can cause liver damage, hair loss and other side effects. It is harmful to a developing fetus and should not be used by women who may become pregnant and are not using appropriate contraception, or their male partner.
- Natalizumab (Tysabri). This medication is designed to block the movement of potentially damaging immune cells from your bloodstream to your brain and spinal cord. It may be considered a first line treatment for some people with severe MS or as a second line treatment in others. This medication increases the risk of a viral infection of the brain called progressive multifocal leukoencephalopathy in some people.
Alemtuzumab (Lemtrada). This drug helps reduce relapses of MS by targeting a protein on the surface of immune cells and depleting white blood cells. This effect can limit potential nerve damage caused by the white blood cells, but it also increases the risk of infections and autoimmune disorders.
Treatment with alemtuzumab involves five consecutive days of drug infusions followed by another three days of infusions a year later. Infusion reactions are common with alemtuzumab. The drug is only available from registered providers, and people treated with the drug must be registered in a special drug safety monitoring program.
- Mitoxantrone. This immunosuppressant drug can be harmful to the heart and is associated with development of blood cancers. As a result, its use in treating MS is extremely limited. Mitoxantrone is usually used only to treat severe, advanced MS.
Treatments for MS signs and symptoms
Physical therapy session
Physical therapy. A physical or occupational therapist can teach you stretching and strengthening exercises and show you how to use devices to make it easier to perform daily tasks.
Physical therapy along with the use of a mobility aid when necessary can also help manage leg weakness and other gait problems often associated with MS.
- Muscle relaxants. You may experience painful or uncontrollable muscle stiffness or spasms, particularly in your legs. Muscle relaxants such as baclofen (Lioresal) and tizanidine (Zanaflex) may help.
- Medications to reduce fatigue.
- Other medications. Medications also may be prescribed for depression, pain, sexual dysfunction, and bladder or bowel control problems that are associated with MS.