3) Rest, Meditation and Prayer

Adequate Rest is cornerstone to managing MS.
Most people with multiple sclerosis (MS) end up dealing, at some point, with fatigue — whether it’s occasional or constant, mild or debilitating. Several different aspects of self-care can minimize fatigue, including budgeting enough time for sleep, getting enough exercise, and following a nutritious diet.
But for most people with multiple sclerosis, fatigue is a symptom to be managed, not entirely prevented — which means that resting is another important aspect of self-care.
There isn’t, of course, any single right or wrong way to rest. What kind of rest you need will depend on your level of fatigue and what factors are contributing to it. But there are certain guidelines you can follow to ensure that you take breaks when you need them the most, and that you get the most benefit possible from them. https://relaxlikeaboss.com/
Meditation
Stress, anxiety and mental fatigue severely worsen symptoms of MS. Due to hormonal changes and other biochemical responses to stress, the nervous system is aggravated, creating pain and depressing the immune response.
Sleep disorders often result causing fatigue which increases one’s susceptibility to stress. This, in turn, exacerbates MS symptoms. Hence a vicious circle gets created.
An effective stress reduction technique, and a key component of Ayurveda, Transcendental Meditation is a program, which is excellent for:
- Reducing and often removing stress altogether
- Removing the stress component of pain
- Reducing insomnia
- Promoting rest and relaxation
- Creating inner peace and enhancing emotional well-being
- Increasing self-awareness
- Reducing negativity and depression
- Reducing fatigue and increasing energy
- Meditation has also been shown to help:
- Reduce symptoms of allergies and asthma
- High blood pressure, heart disease and cancer
- Binge eating, substance abuse and anxiety disorders
Transcendental Meditation is the single most effective tool Richard Beecroft and the Beyond MS Association use to overcome MS – physically, mentally, and spiritually.
Multiple Sclerosis & meditation: Two testimonials
April 23, 2015
Perhaps the most important scientifically proven health benefit of the Transcendental Meditation technique is its positive effect on stress. This is good news to patients diagnosed with Multiple Sclerosis, a condition aggravated markedly by stress and anxiety.
Here are two stories from people whose daily meditation practice makes it easier to live with MS.
Ben’s story
Ben (35) was diagnosed with Multiple Sclerosis. He felt constantly weak and tired, had problems with balance and malaise, and strong spasms in his right leg.
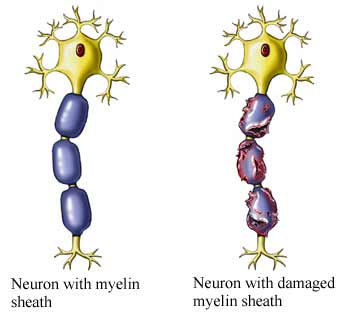
HOW THE DISEASE AFFECTS THE BODY: An illustration depicting a neuron with its myelin sheath intact (left), and one affected by Multiple Sclerosis. The disease damages the myelin sheath and thereby hinders nerve impulse transmissions. Illustration: UVA Health. READ MORE about meditation and MS
As if this wasn’t enough, Ben started to notice aching and loss of vision in his left eye. Knowing that MS can cause lasting damage to the optic nerve, he felt severely depressed and anxious.
Ben was admitted to a hospital in Florida Tests performed revealed abnormalities in spinal fluid and MRI brain scan, which were consistent with his diagnosis of MS.
Upon being discharged from the hospital, his physician advised him that nutritional supplements and dietary approaches would not alter the course of the disease. He was given a prescription for Xanax, a strong tranquilizer with a substantial risk of misuse and dependence.
Three weeks later, he arrived at the Raj Ayurveda Health Center in Fairfield, Iowa — already in a wheelchair.
Initial examination revealed abnormalities of the left eye and optic nerve, abnormal reflexes in both legs, with weakness and lack of coordination in both legs and severe difficulty walking.
Ben underwent a treatment program which included Ayurveda purification, dietary changes, learning the Transcendental Meditation technique, yoga, and specific herbal preparations. By the end of his stay, he could walk 800 yards unassisted.
Nearly twelve years after his first in-residence program, Ben continues to follow the natural approach to Multiple Sclerosis treatment, including his Transcendental Meditation practice, Ayurvedic diet and herbal preparations.
Ben has not experienced any symptoms of relapse; he now walks two miles daily, lifts weights and describes himself as ‘having a positive attitude without depression or anxiety’. His energy level is good and he is working full-time as a massage technician.
Cheryl’s story
Cheryl has had MS for over 30 years. She provides a real insight into how knowledge of the disease has progressed immensely during this time.
 “I was diagnosed in March 1983,” Cheryl recalls. “At the time, I was a marketing assistant at a magazine, in NYC and used an electric typewriter. (You can find them in museums.) One day I noticed that I was making an unusual amount of errors. I also had numbness in my hands and a feeling of an electrical charge down my spine when I bent my neck forward.
“I was diagnosed in March 1983,” Cheryl recalls. “At the time, I was a marketing assistant at a magazine, in NYC and used an electric typewriter. (You can find them in museums.) One day I noticed that I was making an unusual amount of errors. I also had numbness in my hands and a feeling of an electrical charge down my spine when I bent my neck forward.
“There were no MRI’s back then, so diagnosis was made with a mylogram and spinal tap and I spent two weeks in the hospital! My doctor said he thought it was MS but only time would tell.
He gave me steroids to arrest the symptoms. Nine months after my daughter was born in 1985, I lost the eyesight in one eye. I was again given steroids and my eyesight came right back. This time I had my first MRI and was given a definitive diagnosis of MS.
It wasn’t until 1999 that I had another exacerbation (weakness in my legs) while working on a Masters in Divinity at Princeton Theological Seminary that I found another doctor who put me on Avonex. I use Avonex for 3 years, then was switched to Rebif. I just recently started taking Tecfidera because I was running out of injection sites…
I practice Yoga and Transcendental Meditation. This, with prayer, helps with the stressors of work and life in general.
I work out a at gym to keep my muscles strong. I also take a multiple vitamin, vitamin D, cranberry supplements (to keep UTI’s in check) and omega 3 fatty acids daily.
All in all, I can proudly say: “I have MS but MS doesn’t have me!””
Sources:

Between September 2005 and May 2008 in Vicksburg, Mississippi, retired pediatrician Peter Boelens helped people with depression. But he didn't use medicine; he claimed that his cure was prayer. For one hour a week for six weeks, 27 men and women engaged in person-to-person prayer sessions during which they prayed with a Christian minister without making any physical contact. They prayed for forgiveness, and they prayed for god to heal their stresses.
Everyone in the study met the DSM criteria for depressive disorder, and many of them had anxiety too. At the end of six weeks, their self-reported scores on the Hamilton Rating Scales for Depression and Anxiety had all gone down. They also showed increases on a "Life Orientation Test" that tests for optimism and a "Daily Spiritual Experiences Scale," compared to a control group who received no intervention at all.
One year later, when Boelens followed up, the prayer group had maintained their mental health. "You release all the feelings and the emotions," he says. "You dump them out at the foot of the cross and dust them off, and the blood of Jesus washes them away." Last year, Boelens repeated his experiment, wanting to know more. He teamed up with a Baylor College of Medicine neuroscientist Ramiro Salas to see what the brains of the people who prayed were doing.
"I study the brain, not religion," Salas says, when I ask him about the possibility of prayer as a treatment for depression. Salas's work focuses on the mentally ill brain, trying to find ways to predict through imaging what treatments could be most effective. To do that, he designed an experiment for 14 new prayer subjects with depression, all recruited from Houston churches, and asked them to remember their biggest trauma. He scanned them before and after six weeks of prayer with Boelens. Along with their self-reported improvements, Salas found compelling neurological changes: He saw more activity in the prefrontal areas of the brain when he asked them to think about their trauma. This area of the brain is thought to regulate cognitive control, suggesting that "whatever happened during prayer allowed the patient to actually have better cognitive control over their emotions," Salas says.
The precuneus, a region which has been associated with introspection, was less activated when the group was asked to think about their trauma. "What that might mean is that, after prayer, they're feeling that these feelings are not really who they are, they don't define them anymore," Salas says. There are a lot of caveats to their study, Salas says. They only looked at 14 people. The sample group was biased, because they were all recruited from churches, so they were likely to be Christian already. Boelens, Salas says, is a very likeable and charismatic person. "One of my questions is: Is this a Peter-specific effect?' Salas says. "If Peter says after six weeks, 'Do you feel better?' and you really like Peter, you're going to tell him, 'Yes Peter, I feel better.'"

Salas says they need to repeat the study, and have people pray with someone else, test other religions, and a variety of degree of beliefs. "There's so many things we should do," he says. "Basically, the experiment we did shows that if you're a Christian, and you're depressed, and you pray with Peter for six weeks, your brain changes, and you claim that you're a lot better. But that's still something that should be studied."
https://tmhome.com/benefits/tm-helps-patients-with-multiple-sclerosis/
https://tmhome.com/benefits/multiple-sclerosis-meditation-a-case-study/